Standardizing clinical data yields manifold benefits throughout the research lifecycle. Primarily, it bolsters data quality by mitigating errors and inconsistencies stemming from varying data formats and definitions. This uniformity fosters interoperability, easing data sharing and collaboration among diverse organizations and systems.
What Are CDISC and SDTM?

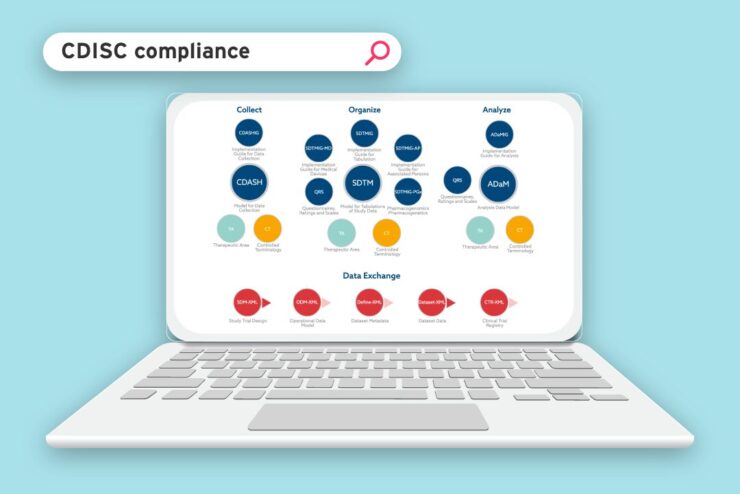
Clinical Data Interchange Standards Consortium (CDISC) streamlines the collection, exchange, and submission of clinical research data by developing standards. Study Data Tabulation Model (SDTM), on the other hand, is one of its standards, providing a structured format for organizing clinical trial data. This facilitates regulatory review by the Food and Drug Administration and the European Medicines Agency.
SDTM fosters collaboration among stakeholders and guarantees data reliability and compatibility. Adhering to SDTM guidelines enables seamless data integration and analysis, enhancing the efficiency of clinical research processes.
In this guide, we delve into why CDISC and SDTM datasets matter, how they impact clinical research, and what their role is in shaping the future of healthcare.
Benefits of Standardized Clinical Data
Standardized data streamlines regulatory compliance by ensuring conformity with stringent requirements of regulatory bodies such as the FDA and EMA. This expedites regulatory reviews and enhances transparency and accountability in clinical research.
When clinical data is standardized, it becomes easier for researchers to analyze and understand it quickly. This means they can make decisions faster based on the information they have.
Also, standardized data allows different types of information, like electronic health records (EHRs) and real-life evidence (RWE), to be combined smoothly. This helps researchers get a better overall picture of diseases and how treatments work. You can visit this website to learn more about the importance of SDTM.
Examples Of CDISC SDTM Datasets

CDISC SDTM datasets typically include data collected during clinical trials, organized into standardized domains. Some common SDTM domains include:
1. Demographics (DM)
This domain contains demographic information about the study participants, such as age, sex, race, and ethnicity.
2. Adverse Events (AE)
This domain includes information about adverse events reported during the study, such as the event type, severity, start and end dates, and relationship to the study treatment.
3. Concomitant Medications (CM)
This domain contains data on medications taken by study participants during the trial, including the medication name, dosage, start and stop dates, and indication.
4. Vital Signs (VS)
This domain includes measurements of vital signs collected during the study, such as blood pressure, heart rate, temperature, and respiratory rate.
5. Laboratory Tests (LB)
This domain contains results from laboratory tests performed during the study, such as blood chemistry, hematology, and urinalysis.
6. Medical History (MH)
This domain includes information about the medical history of study participants, such as past medical conditions, surgeries, and hospitalizations.
7. Findings About (FA)
This domain includes findings related to the study objectives, such as efficacy endpoints, disease assessments, and clinical trial outcomes.
How To Implement CDISC and SDTM

Implementing CDISC and SDTM requires several key steps to ensure effective adoption and integration into an organization’s existing processes. These steps include:
1. Assessment and Planning
These are key for CDISC and SDTM implementation. Assess current practices and create a comprehensive plan outlining the necessary goals, timelines, and resources. This ensures improved data quality and streamlined processes.
2. Data Mapping and Transformation
It involves aligning existing data elements with SDTM standards and converting raw data into an SDTM-compliant format. This ensures accurate categorization and standardization of clinical trial data, which is essential for adherence to CDISC standards and regulatory requirements.
3. Documentation and Training
Document SDTM implementation procedures, including data mappings, transformation rules, and validation criteria. Train staff members involved in data collection, management, and analysis to ensure compliance with CDISC standards and best practices.
4. Validation and Quality Assurance
Implement validation checks to ensure the accuracy, completeness, and consistency of SDTM datasets. Conduct regular quality assurance audits to identify and address any issues or discrepancies in the data.
5 Regulatory Submission
Regulatory Submission requires preparing SDTM datasets to meet CDISC and regulatory standards. This ensures compliance and expedites the review process for new therapies and treatments.
Tips When Implementing CDISC and SDTM

Implementing CDISC standards, including SDTM, in clinical trials necessitates careful planning and following best practices. Here are some tips for successfully implementing CDISC and SDTM:
1. Understand CDISC Standards
Gain a thorough understanding of CDISC standards, including SDTM, by reviewing official documentation, training materials, and resources available on the CDISC website. Familiarize yourself with the structure, domains, variables, and implementation guidelines.
2. Plan Early
Incorporate CDISC implementation early in the clinical trial lifecycle. Integrate CDISC standards into study protocols, case report forms (CRFs), data management plans, and other relevant documents from the outset.
3. Engage Stakeholders
Collaborate with key stakeholders, including clinical researchers, data managers, statisticians, regulatory affairs professionals, and IT specialists, to ensure alignment and buy-in for CDISC implementation. Involve stakeholders throughout the process to address concerns and gather feedback.
4. Standardize Data Collection
Design CRFs and data collection instruments following CDISC standards and guidelines. Use standardized terminology, coding systems (e.g., MedDRA for adverse events, LOINC for laboratory tests), and controlled vocabularies to ensure consistency and interoperability.
5. Implement Data Management Processes
Establishing robust data management processes ensures the collection, validation, cleaning, and transformation of clinical trial data according to CDISC standards. Develop data validation checks, edit checks, and quality control procedures to detect and resolve errors or inconsistencies early.
6. Utilize CDISC-compliant Tools
Select and use data management and analysis tools that support CDISC standards, including electronic data capture (EDC) systems, clinical trial management systems (CTMS), and statistical analysis software capable of generating SDTM datasets and adhering to CDISC guidelines.
7. Train Personnel
Provide comprehensive training to personnel involved in CDISC implementation, including clinical investigators, study coordinators, data managers, and statisticians. Ensure staff members understand CDISC standards, data collection procedures, and management practices.
8. Conduct Validation and Compliance Checks
Perform validation and compliance checks to verify that SDTM datasets conform to CDISC standards and guidelines. Use validation tools, rules, and checks to assess quality, completeness, and compliance.
9. Document Thoroughly
Maintain comprehensive documentation throughout the CDISC implementation process, including study protocols, data management plans, validation plans, SDTM specifications, and compliance documentation. Document decisions, processes, and deviations to facilitate transparency, reproducibility, and regulatory compliance.
Future Directions and Challenges

Even though there have been some good advancements, there are still obstacles to getting everyone to use CDISC and SDTM standards widely. The obstacles involve insufficient resources, navigating complex technicalities, and resisting organizational change.
To tackle these challenges, it’s crucial for all parties—researchers, organizations, regulators, and industry bodies—to collaborate. We must invest in training, enhance infrastructure, and secure continuous support from regulatory agencies. By taking these steps together, we can unlock the power of standardized clinical data to push medical research forward and improve patient care.
Conclusion
Standardizing clinical data with CDISC and SDTM datasets is vital for advancing research, improving patient outcomes, and ensuring the integrity of clinical trial data. Following CDISC standards and using the SDTM framework makes it easier to manage data, improves its quality, helps different systems work together, and speeds up the development of new therapies and treatments. Embracing data standardization remains crucial for driving innovation and transforming healthcare in an evolving landscape.

